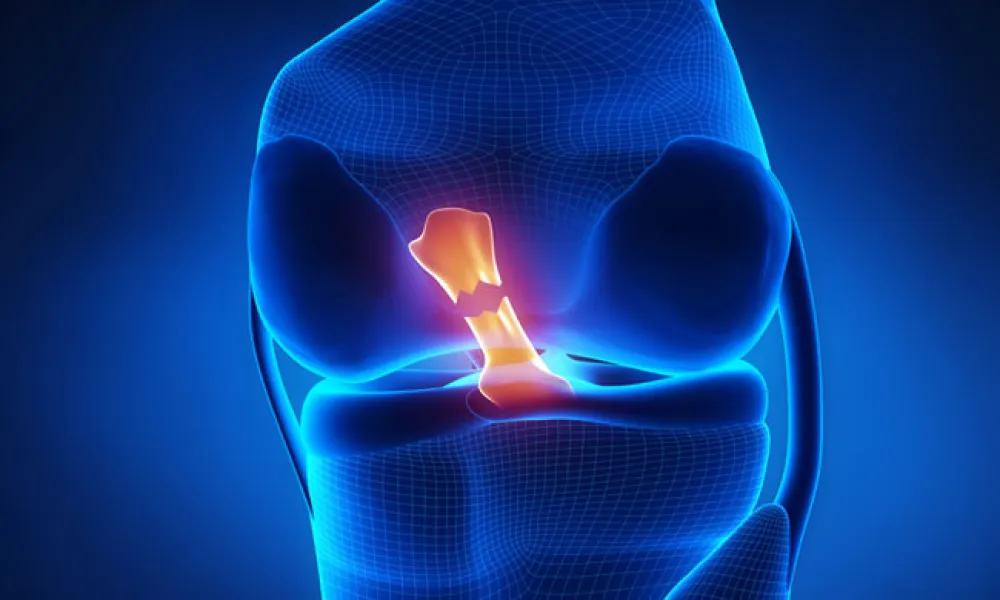
If you schedule an ACL Reconstruction. The Anterior Cruciate Ligament (ACL) is a major knee ligament. Injuring the ACL can cause instability, which might injure other knee structures. The original ACL injury often coincides with injury to meniscus cartilage. Surgery for ACL tears involves reconstructing the ACL to restore knee stability.
The tissue that replaces the ACL is often borrowed from another part of the knee, (donated tissue can also be used). Portions of your hamstring tendons are sometimes used. The operation is arthroscopic, allowing the surgeon to view the entire knee with small incisions. A marginally longer incision is made to obtain tissue or the graft to be used in ligament reconstruction. Tunnels are made in the bones on either side of the knee joint. Tissue grafts are anchored on each bone and the anchoring devices remain permanently.
Ideally, the graft heals to the bone and after a year, the bond is as strong as the original ACL. A femoral nerve block is offered to decrease your pain post-surgery. Immediately following surgery, your leg will be weak because of the nerve block. Post-surgery patients use crutches for 24 hours and then as needed. Patients may use crutches longer if other injuries occurred with the original ACL injury.
Your knee will be swollen post-surgery. Your physician can prescribe medications to control your pain. Rest, ice, and anti-inflammatory medication and rest will decrease the pain. Most patients walk without crutches within four weeks. After 8-12 months, patients regularly return to cutting-type athletic activities. Rehab is important to recovery. Surgeons often suggest that patients participate in physical therapy.
- The process before surgery.
- Decision to have the operation.
- Discussing questions and concerns with a surgeon.
- Our authorization secretary contacts your insurance to let you know how much of the bill your insurance will cover.
- Once you are authorized, you choose a date. You should have full motion of your knee pre-surgery. Physical therapy is often recommended prior to the operation.
- Arrange for family or friends to assist you on the day of surgery, and when you get home. You are not allowed to drive yourself home.
- Schedule your physical therapy and post-surgery visit with your surgeon’s physician assistant)
- We recommend you stop birth control 2 weeks before surgery and 4 weeks after surgery.
- Risks
Your surgeon considers the risks and potential complications, as well as the benefits and anticipated outcomes before recommending an operation. There is a less than a 1% risk of infection. There is a less than a 1% risk of major nerve injury. Many patients do develop a numb patch on their leg near the incision. Numb areas often shrink in size within six-months post-op. However, some persist permanently. You have a 3% chance of developing a DVT (deep vein thrombosis – a blood clot). Surgeons will question you pre-operation to help you understand and decrease DVT risk. You will be given instructions to help avoid DVT post-surgery. There is a rare (less than 1 in 200,000) chance of loss of life or limb.
- Routine follow up:
- 7-14 days with the phys. assistant for a wound check.
- At this point, paperwork for missed work, disability, school, and PE notes are completed.
- 6 weeks with the doctor
- 3 months with the phys. assistant for progress check
- 6 months with doctor for exam and possible release to increased activity.
Links
AAOS (American Academy of Orthopedic Surgeons) Sports Injuries